Ever wondered about your Pelvic Floor?
It’s a funny thing when we discover that we have been wrongly conditioned to believe something about ourselves. And for me, that belief was actually about my Pelvic Floor!
Having a weak pelvic floor was something that had become so ingrained in me that in many ways it impacted how I trained, how frequently I was doing my pelvic floor exercises (too often!), as well as the frequency I was going to the bathroom pre-workout or long drive!
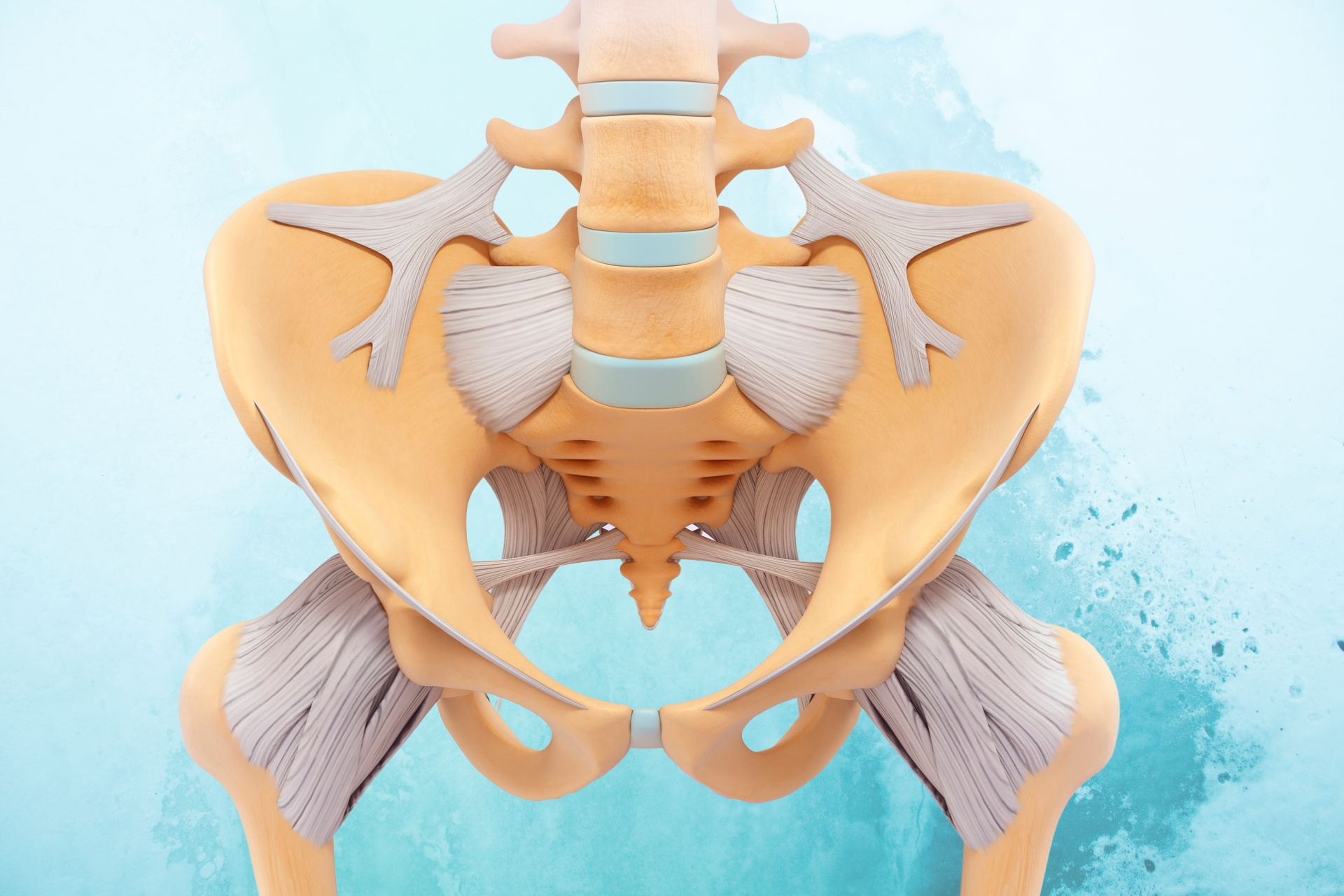
As an Exercise Physiologist and Running Coach, Pelvic floor (PF) and core stability is a topic I discuss with clients, literally on a daily basis and almost exclusively the topic of ‘strengthening’ and training the pelvic floor (PF) complex. Despite being in the Health and Fitness Industry for over 20 years it has only been in recent months the concept of an ‘overactive pelvic floor’ has hit my radar and how it can affect your pelvic stability. You see, the majority of fitness professionals are trained and conditioned to believe the PF complex will be weak in almost everyone you see and all the cueing and information we are taught at uni and beyond is on how to work it in one direction - up! Lift, hold, count, repeat. We are always encouraging clients to hold in that wind, stop the flow of urine, to master the gold standard 10-second endurance hold. There was no consideration that these muscles could be overworked or could get stuck in a state of almost constant contraction! Naturally, if a muscle is already contracted there will be very little movement on assessment and thus presumed to be weak or underactive.
On reflection, there has been one occasion when I discovered the importance of being able to relax that pelvic floor and that was when I had a Physio assessment during my pregnancy back in 2018. During that appointment, I remember the Physio mentioning that “it would be a good idea to practice relaxing my PF as the chance of a tear during birth and long-term issues postpartum will be high. To be honest I don’t remember much in the way of technique instruction and really just tried to ignore the underlying fear I now had while I practiced a technique with no idea if I was doing it effectively. This fear became so ingrained in me that when I woke from the General Anaesthetic post-C-Section birth (it's a long story!!) my first memory is of doing my PF lifts. True story. I had gotten myself in quite a state about it and had secretly panicked about the birth for the remaining months of pregnancy. All the while I silently pleaded with these PF muscles to relax while no doubt clenching the crap out of them in my stress state!
While this physio had in fact suggested the concept of relaxing these incredible muscles it was only provided in the context of being important during birth. Similarly, when I had my assessment post-birth by a different physio I was told my PF “wasn’t great, but it likely never had been” so continue with the daily PF endurance holds, bounces and glute squeezes. Sound familiar to anyone?
Now I am at no point suggesting these Physio’s did the wrong thing because I’m also a trained professional and I never questioned it either. I just continued believing that I was like many women - weak through the PF, that my years of running, endurance training and overzealous toileting habits had likely made it worse. I also didn't start to connect the dots that the niggling pelvic, tailbone, hip and glute injuries that started to occur within 6 months of birth may have been due to anything other than my own pelvic structure and hormones changing.
What I am suggesting is that knowledge is power and that it is important to consider all that is going on rather than make a presumption that weakness of the PF is the only option.
So here I am some hours after my appointment at Pelvic Health Melbourne feeling a combination of relief, direction, focus, awe, and just a little bit of frustration and embarrassment that I didn’t know all this sooner. So why did I book in for a Pelvic Health Assessment four years postpartum with no apparent PF issues or symptoms? Initially, the idea was solely to go for my own learning and development and to find out exactly what I would be referring my clients for!
With a lot of PD occurring in the background of my life with a particular focus on Women’s Health it was only natural that I would start to link my learning to clients I was seeing and as fate would have it just recently I had been referred a patient who had torn a PF muscle during exercise due to it being hypertonic (muscle tightness/ increased tone). The more I read and researched in recent weeks the more I started pondering my own long-term hamstring and hip issues, particularly since having my daughter. By the time I arrived at my appointment I was almost excited to get confirmation that it was my pelvic floor causing a lot of my injury issues that despite long-term rehab would not go away.
Again I will re-state - Knowledge is Power and in my appointment today I saw via Real Time Ultrasound and as well as a complex examination that my previous conditioning and belief were all wrong. My left side pelvic floor musculature is basically locked on and when attempting the lifts and holds it barely moves from its already elevated state. Because of this over-active muscle, the rest of my pelvis is being pulled in odd directions and it gives reason and explanation to almost every niggly injury and irritation that has presented over the past four years. It also explains why on many occasions I’ve struggled to pinpoint exactly where the pain was originating from… turns out I was trying to find it on the outside of my pelvis when all the while it was on the inside.
So now I have a different type of rehab ahead of me, getting the muscles to release and relax using a combination of pressure release work and belly breathing techniques to encourage the pelvic diaphragm to work effectively.
So to wrap up and provide you with some practical takeaways…
- If you haven’t had a complex and in-depth Pelvic Health Assessment then book in now! Honestly, it is worth it. Pelvic pain, incontinence, instability, unexplained injuries, and prolapse are all treatable and they are surprisingly common, it's just that we don't talk openly about our issues!
- I 100% recommend Pelvic Health Melbourne and if there isn’t one near you they can advise on who to see in other areas. Email: info@pelvichealth.melbourne
- If something doesn’t feel right for you or you have a chronic or ongoing niggly injury that won't rehabilitate, ask questions, think outside the box and follow your intuition. Don’t settle or ignore it and hope it will go away!
- If you had a C-Section you still need to be assessed! And if you are male you too may need to be assessed. Everyone can experience Pelvic Health issues.
- PF training should involve mastering both relaxations as well as contractions. It is not just about contracting and holding.
- Finally and somewhat shockingly Bluey, or more specifically Bandit was wrong about this. A tactical wee is actually not a good idea in the long term and can cause a number of issues. Crazy I know!
If anything in this blog resonates with you please reach out and ask any questions you have.
I am in no way affiliated with Pelvic Health Melbourne, nor do I receive any compensation or reward for recommending them. This is my honest opinion of the treatment I have received and I couldn’t be more impressed.
Blog re-posted with permission from Kylie Royal Meehan from Fit Well You. https://www.fitwellyou.com.au
Thank you Kylie

Kylie Royal Meehan - Fit Well You
A little about Kylie
Kylie is an advocate of wellness in every sense of the word!
Her passion for anything health, fitness and wellness is like a beacon but she also has a strong belief in balance and making the most of life’s opportunities!
Kylie has been in the industry since the late 90’s working as an Exercise Physiologist and Personal trainer as well as in high-level injury rehabilitation, with elite athletes at the AIS and NTIS and with the general population.
Kylie's aim is that her positive attitude and high level of motivation will rub off on her clients and they will live their best lives.
Qualifications: Accredited Exercise Physiologist, Level 2 Recreational Running Coach, Personal Trainer.
Mental Health First Aid trained and Peer Support leader (Emergency services sector).
More from the blog







